Genetics & COVID-19: What You Need To Know
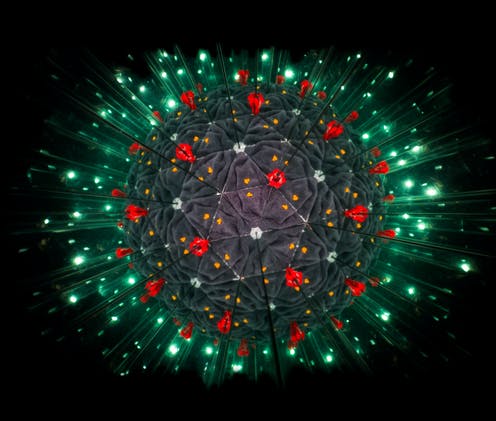
Photo credit: https://theconversation.com/heres-how-scientists-are-tracking-the-genetic-evolution-of-covid-19-134201
October 16, 2020
The spread of COVID-19 has already been discussed on multiple occasions. With that, many people came together to find ways to protect us from this sometimes fatal virus. Governors and state regulations made it mandatory that businesses and restaurants either close down completely or make wearing masks mandatory. Businesses created capacity limits, six feet-apart signs, and made sure to sanitize areas exposed to human contact. However, the virus is still spreading pretty quickly, and as scientists scatter to find a new vaccine, a new factor of the virus has come into play: genetics.
Researchers have tied COVID-19 severity and susceptibility to some genes associated with the immune system’s response, as well as a protein that allows the disease-causing SARS-CoV-2 coronavirus into our cells. They have also found some information that links to the probability that Blood Type may be a factor when it comes to the person’s ability to catch the virus. The effects of social and economic inequalities that also increase risk and tend to be concentrated in populations with specific ethnic backgrounds and ancestries.
Priya Duggal, director of the genetic epidemiology program at the Johns Hopkins Bloomberg School of Public Health believes that separating the genetics from the inequalities increasing risk could be very beneficial.
“We don’t want that to be conflated,“ she says. “Race is representing many factors, including people who are essential workers” and may be routinely exposed to more chances of infection because of their job or who may not have good access to health care. “These are things we have all known to have existed in this country for a long time, and COVID-19 just brings them right to the front.” says, Duggal.
A significant peer-reviewed genetic studies to date, published on June 17 in the New England Journal of Medicine, relied on two European populations. In that study, researchers picked through the genomes of 1,610 hospitalized patients in Italy and Spain to find DNA changes that were common among people with COVID-19 respiratory failure. The investigators found many patients with severe disease had variants in a complex of genes on chromosome 3. Proteins called Chemokines were found in these genes.
Chemokine’s purpose is to serve as a chemical bait that lures immune cells to tissues under attack, and allows them to destroy infected cells. But under observation, it seems that Chemokines go into overdrive and trigger assaults that destroy the lungs when dealing with coronavirus. This key variant seemed to be found 1.5 times more in patients who rely on a ventilator rather than people who use a milder form like supplemental oxygen. Many researchers are saying that this small change will help regulate Chemokines. Although, severely affected patients with two copies of this variant were somewhat younger than those with one or no copy, suggesting that a double dose trumped some of the protective benefits of younger age.
The researchers in the New England Journal of Medicine study also found an association with chromosomes that determine blood type. The study showed that people with blood type A had a 1.5 more likely chance of having respiratory failure than people with other blood types. Other studies published also state that blood type A is also at a higher risk at contracting coronavirus than blood type O. However, the information about the blood types isn’t completely certain, and there are still some factors that could explain the result of these findings.
“Of these genetic findings, the region on chromosome 3 seems to have the strongest association with disease severity”, says Andrea Ganna, a group leader at the Institute for Molecular Medicine Finland
Moreover, there are still more studies and tests that need to be done in order to claim anything is for certain. In the meantime, everyone can do everything they need to be safe for the coronavirus until we find more information to put the virus to a halt.


















